Is your gut health linked to your mental health?
“Is your gut microbiome the key to health and happiness?” ran The Guardian headline in 2017. “Germs in your gut are talking to your brain,” declared the New York Times in 2019.
Your microbiome—the ecosystem of bacteria, viruses, yeast, and other microbes living in your gut—may be sending signals to your brain that alter your mood, your behavior, and your nervous system’s vitality.
“It sounds a bit like science fiction, doesn’t it?” says Valerie Taylor, head of the department of psychiatry at the University of Calgary.
She’s talking about evidence that microbes in your gut may influence your brain. For example:
- Mice are anxious and prefer dark, enclosed spaces. But if they’re born and raised without gut microbes, they freely scurry around light, exposed areas.
- When microbe-depleted rats get fecal transplants from people with severe depression, they act more sad and anxious than rats that get transplants from people without depression.
- Other research hints that the microbiome may play a part in autism, Parkinson’s, and more.
But there are enormous gaps in what we know. For one thing, the research has largely been done on rodents.
“Those rodent studies have advanced our understanding of the microbiome-gut-brain axis, but we don’t know what the results mean for people,” notes John Kelly, a lecturer in clinical psychiatry at Trinity College Dublin.
“In most cases, you can’t compare what’s going on in a mouse with a human,” says Gregor Reid, professor of microbiology and immunology at Western University in Ontario. “We’ve cured cancer many times in mice.”
Here’s what researchers know…and what they’re still trying to figure out.
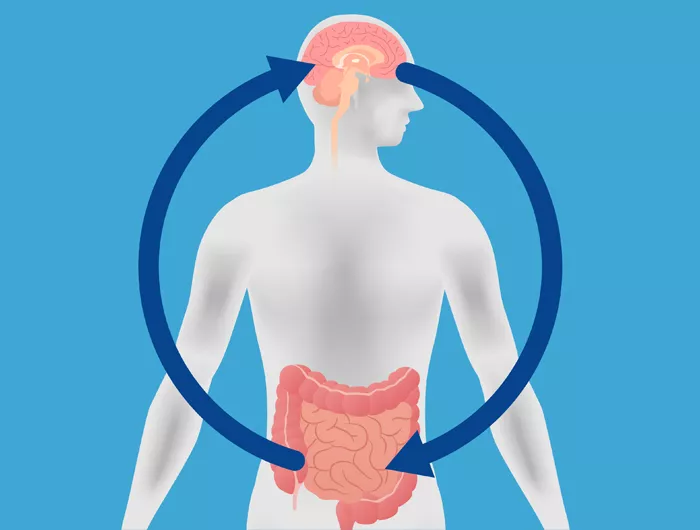
Your gut & brain are talking

Ever had “butterflies” in your stomach? That’s the chatter between your brain and your gut. And some of those signals may come from microbes.
“But no one’s exactly sure how gut bacteria are communicating with the brain,” says Taylor.
Some possibilities: bacteria may send signals through the vagus nerve, which runs from the brain to the abdomen. “Microbes may also talk to the brain via hormonal mechanisms, like by altering the stress hormone cortisol,” Taylor explains. “And gut bacteria may influence inflammation, which could have an impact on brain functioning.”
What’s more, she adds, “some bacteria produce neurotransmitters like serotonin and dopamine, which help regulate mood and affect mental illnesses like depression and bipolar disorder.”
But that’s in the gut. “Do those neurotransmitters even get to the brain?” asks Reid. “If so, are they having an influence? Are they reducing anxiety? We don’t know.”
It’s time to do those studies, and not just in rodents, says Reid. “Researchers can publish all the mice data they want, but until they do something in humans, I’m not sold.”
So far, most human studies have merely observed that people with disorders like depression, bipolar, autism, and Parkinson’s have different microbiomes than people without those disorders.
In the best study, researchers analyzed gut bacteria in roughly 2,100 Belgian and Dutch adults.
“Two types of bacteria were depleted in people with depression, even after taking antidepressant use into account,” says Kelly.
But the cause and effect aren’t clear. Did the missing bacteria cause depression? Or are they missing because depressed people eat differently or are different in some other way? This kind of study can’t say. And it certainly can’t prove that restoring the depleted bacteria will lift depression.
The bottom line
“There’s room to be optimistic that microbes could play a role in mental health,” says Reid. “But I’m trying to give people a reality check.”
That reality: large, well-designed trials haven’t demonstrated that the microbiome affects the brain.
“It’s good to be excited about this area of research, but it’s best to be cautious and not waste your money on supplements that make claims about mood or mental health that the science doesn’t support,” says Taylor.

