The heart of the matter

Which foods protect your arteries?
"Replacing saturated fat with healthier fat could lower cardiovascular risks,” announced a Presidential Advisory from the American Heart Association in July. We talked to the advisory committee’s chair.

Frank Sacks is professor of cardiovascular disease prevention at the Harvard T.H. Chan School of Public Health and professor of medicine at Harvard Medical School. He has led groundbreaking clinical trials on diet and blood pressure, lipids, and weight loss. Sacks spoke with Nutrition Action’s Bonnie Liebman.
The case against sat fat
Q: How strong is the evidence that saturated fat in foods like meat, butter, and cheese is harmful?
A: The evidence that saturated fat causes atherosclerosis and heart disease is compelling. It’s consistent across randomized trials, large observational epidemiologic studies, and animal studies.
Saturated fat increases LDL—or low-density lipoprotein—cholesterol. And LDL cholesterol is a cause of heart disease. It’s not a risk factor. It’s a direct, absolute cause.
It all fits very, very well. And that builds a powerful case that saturated fat causes heart disease, and it is healthful to replace it with unsaturated fat, especially polyunsaturated fats like those in soybean oil, mayo, nuts, and fish.
Q: Why have some people heard that the evidence on saturated fat has gotten weaker?
A: Some of the more recent studies take a standard epidemiologic approach, which is inadequate. Saturated fat seems to be harmless in those studies because it’s being compared, by default, to the typical American diet, which is high in refined, junk-food carbohydrates. They’re also linked to a higher risk of heart disease.
Q: Why inadequate?
A: Let’s say you give someone advice to reduce their saturated fat. Well, what do they eat instead? If they just reduced their saturated fat, they’d lose weight, because they’d be getting fewer calories. That’s unlikely. So what do they actually do? In many cases, people who eat less saturated fat eat more refined carbohydrates.
Q: Like white bread, pasta, rice, sweets, and sugary drinks?
A: Yes. But Walter Willett and Frank Hu—my colleagues at Harvard—devised a new epidemiology based on food substitutions that would occur in real life. And that’s really innovative.
Q: Because they look at what’s replacing the saturated fat?
A: Yes. They’ve designed a method where, with everything else being equal, they can compare people who have, say, high saturated and low unsaturated fat intakes with people who have low saturated and high unsaturated fat intakes.
When they do that, it’s clear that higher saturated fat and lower unsaturated fat is a bad dietary pattern.
Q: Can a lower-fat diet be healthy?
A: Yes, if the foods are healthful, such as whole grains, vegetables, fruits, and beans. But not if they’re rich in refined, junk-food carbohydrates.
Q: Didn’t you re-examine the clinical trials from the 1960s that assigned people to diets with different fats and then measured heart disease rates?
A: Yes. We separated them into core and non-core trials, because some were superb in quality, and some were kind of dreadful. So we set out uncontroversial criteria for a good clinical trial.
For example, core trials had to keep people on diets for at least two years and had to use a biomarker like blood cholesterol to show that people were sticking to their assigned diets.
Q: What did the core trials find?
A: The risk of heart disease was about 30 percent lower in people who ate polyunsaturated fats instead of saturated fats. If you include the non-core trials, you see only about a 20 percent lower risk of heart disease, but that is still statistically significant.

Source: Adapted from “The Facts on Fat,” American Heart Association.
Photos: Jen Urban/CSPI (left), Kate Sherwood/CSPI (right).
LDL & beyond
Q: How do we know that LDL cholesterol causes heart disease?
A: We know that LDL is the main carrier of cholesterol in the blood, and it enters into the walls of major arteries and deposits cholesterol there. And that sets off a chronic inflammatory reaction, which helps lead plaque to build up in arteries.
Also, people who inherit genes that raise their LDL have a higher risk of heart disease. That’s not true for people with genes that lower HDL, which is sometimes called good cholesterol.
And pretty much any class of drugs that reduces LDL—like statins, ezetimibe, PCSK-9 inhibitors, or resins like cholestyramine—also reduces heart disease.
Q: How do the drugs work?
A: They vary, but statins and PCSK-9 inhibitors increase the number of LDL receptors. Many people have high LDL levels because they have too few LDL receptors, which clear LDL from the blood.
Q: Is large LDL safer than small LDL, as some people argue?
A: No. It’s basically a non-issue. If you have a lot of big LDL, it’s no better than a lot of little LDL. In fact, big LDL is probably worse, because it’s loaded up with more cholesterol.
Q: Do high triglyceride levels cause heart disease?
A: We don’t have proof with triglycerides the way we have proof that LDL cholesterol causes heart disease. But the evidence linking triglycerides to heart disease is getting stronger.
A high level of triglycerides means a high level of VLDL— very-low-density lipoproteins. Like LDL, VLDL can get into the artery wall, deposit cholesterol, and set off an inflammatory reaction.
And Apo C-III, a protein that’s part of VLDL, damages the artery wall.
But triglycerides have less influence on heart disease than LDL cholesterol. That’s partly because VLDL carries much less cholesterol.
Q: Is low HDL a risk, since HDL takes cholesterol out of arteries?
A: We know that people who have low levels of HDL cholesterol have higher rates of heart disease. That’s incontrovertible. As a risk factor, it’s totally solid.
But if you raise HDL levels, can you increase cholesterol removal from the artery wall and reduce heart disease?
That’s where the HDL story breaks down. We’ve got several instances where that doesn’t occur.
Q: HDL-raising drugs haven’t protected against heart disease?
A: Right. HDL is a hot area of research. We’re in the early stages of trying to understand it. My lab is focused on HDL because there’s so much to learn.
WHICH FATS ARE BEST?
Q: Why recommend polyunsaturated fats over monounsaturated fats?
A: The data are stronger for polyunsaturated fats—not just the omega-3 fats in fish oil but the omega-6 fats in soybean and other oils—than for the monos in olive oil and canola oil. [See “Oil in the Family”] And polyunsaturated fats lower LDL more than monos and have anti-inflammatory effects.
Q: What about coconut oil?
A: Coconut oil comprised about 3 percent of the American Heart Association’s advisory and generated about 95 percent of all the press coverage and criticisms. But the evidence is straightforward.
Some of the short-chain saturated fatty acids in coconut oil don’t raise LDL cholesterol. But they don’t counteract the effects of the oil’s longer-chain fatty acids, which do increase LDL cholesterol. So coconut oil raises LDL cholesterol in the same way that, say, butter does.
Q: Have large trials tested coconut oil’s impact on heart disease?
A: No. So, in the absence of any 10,000-person study, we have to go on the best available evidence, which shows that coconut oil raises LDL cholesterol. Coconut oil has no demonstrated benefits to offset the rise in LDL.
Q: What about dairy fat?
A: Butter increases LDL cholesterol just as you’d expect from its saturated fat. It’s like coconut oil, except there’s a lot more data linking dairy fat to heart disease because it was pitted against polyunsaturated fats in clinical trials. And dairy comprises much of the fat eaten by people who have a high saturated fat intake.
Q: How can people avoid confusion?
A: If you want to sort out what is good scientific knowledge and what is speculation or biased, look at guidelines produced by the American Heart Association, American Diabetes Association, or American Cancer Society.
Those well-established organizations carefully vet their advice. Individual studies that have contrarian implications don’t come close to the scientific merit of their advice and guidelines.
For the media, established knowledge is boring. The media wants something new. But that’s not necessarily good for your health.
You’re better off with established scientific knowledge, and if it’s boring, that’s fine. You won’t be healthier because the media sells more newspapers.
Not just the fats, ma'am
Want to protect your heart? It’s not just a matter of eating good fats.
One of the healthiest diets—endorsed by the American Heart Association, the American College of Cardiology, and other health authorities—is called DASH (Dietary Approaches to Stop Hypertension).
A DASH-style diet is low in saturated fat, sugar, and salt, and rich in fruits and vegetables. (It’s also rich in nutrients like potassium, magnesium, calcium, and fiber.)

In 1997, a landmark study, coauthored by Frank Sacks, found that a DASH diet could lower blood pressure as well as some prescription drugs. That news was a bombshell, because high blood pressure (hypertension) is a major risk factor for heart attacks and strokes.
One out of three adults have high blood pressure, and another one out of three have pre-hypertension. Blood pressure creeps up with age, so your lifetime likelihood of having hypertension is 90 percent.
Then, in 2005, came another news flash: The OmniHeart study reported that two variations of the DASH diet were even better than the original:
- The higher-protein variation replaced some of DASH’s carbs with protein—half from plant sources (like beans, peas, and nuts) and half from animal foods (like fish, lean poultry, and low-fat dairy).
- The higher-healthy-fat variation was a Mediterranean-style diet. It replaced some of DASH’s carbs with healthy fats like oils, salad dressing, mayonnaise, nuts, fatty fish, and avocado. (The oils—like canola, olive, and soybean—were polyunsaturated or monounsaturated, not saturated like coconut or palm.)
The two OmniHeart diets beat the original DASH diet because they were better at lowering LDL (“bad”) cholesterol and triglycerides.
We have created a hybrid of the two OmniHeart diets, with a “wild card” that lets you eat one extra serving of carbs, protein, or healthy fat each day. (See “DASH, in a Dash”.) Compared to what most people eat, it has:
- MORE fruits and vegetables,
- LESS red meat, and
- LESS sugar and white flour.
Not eager to start counting servings of this or that? Fill half your plate with fruits and vegetables, shrink the unhealthy carbs, replace fats (like butter) with oils, and cut back on salt. That’ll get you most of the way there.
Photo: Jennifer Urban/CSPI
DASH, in a dash
A DASH-like diet can help lower your risk of a heart attack or stroke. Here’s a 2,100-calorie version. (Note: The serving sizes are small.)

Photos: fotolia.com (top to bottom)— © EWA BROZEK, © Stefanie Leuker, © angelo.gi, © Krzysiek z Poczty, © cultureworx, © Paylessimages, © pockygallery11, © cultureworx
Oil in the family
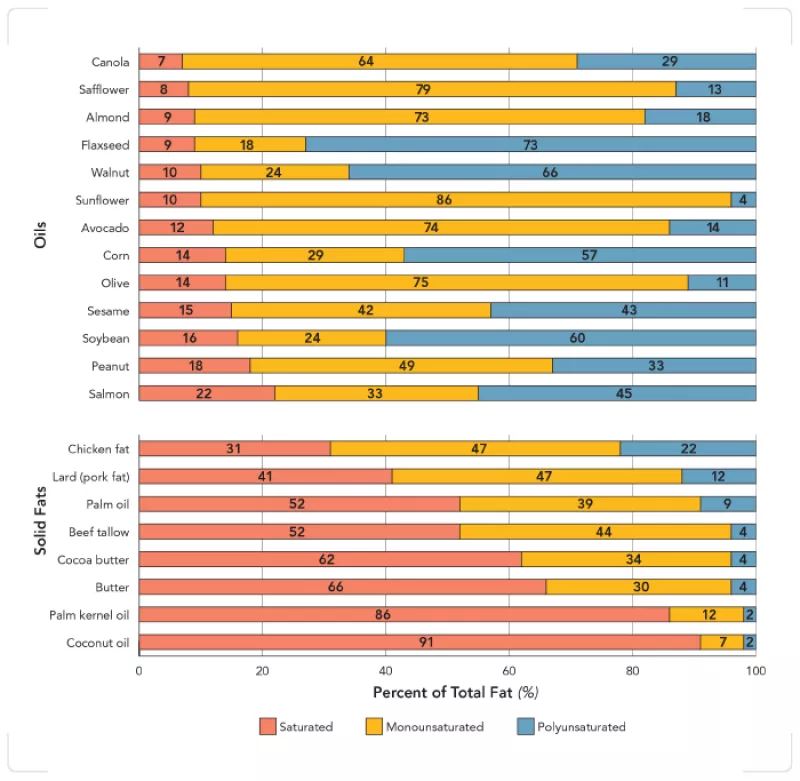
All fats are a mix of saturated, monounsaturated, and polyunsaturated fatty acids (though people usually categorize each by the fatty acid that predominates). Odds are, you get mostly soybean oil in prepared foods (like salad dressings, mayonnaise, and margarine) and restaurant foods. So you’ll probably end up with a good mix of unsaturated fats if you use canola oil and olive oil (when you want its flavor) for cooking.
*Sunflower seeds are higher in polyunsaturated fat and lower in monounsaturated fat than most sunflower oils. Some health food stores sell high-poly sunflower or safflower oils.
Note: The fatty acids in meats, nuts, chocolate, and other foods are similar to their respective oils, butters, etc., shown above.
Sources: USDA National Nutrient Database for Standard Reference (Release 28), National Sunflower Association, Flax Council of Canada.

